Good vs. Bad MovementsBefore delving into the Cat/Cow movements, it is important to think about the construct of 'good versus bad exercises' in general. In my opinion, there are not many examples of inherently bad exercises that are commonly prescribed during a therapy session. If an exercise addresses a patient's impairments, it is likely a beneficial movement. However, I often see good exercises being poorly executed and prescribed. When teaching my patients about their corrective movements, I always emphasize quality over quantity of motion. A good exercise is any movement that addresses the patient's impairments, minimizes pain, and is performed correctly. Cat/Cow Exercise: How It Should Be PerformedCat/Cow is a good exercise! I believe it is good because of it's simplicity. However, it is often performed incorrectly, which significantly diminishes it's effectiveness. The purpose of Cat/Cow is to mobilize the spine and pelvis & retrain spinal movement patterns. When moving into the Cat exercise (Left picture), the entire spine should round, creating a uniform spinal curve. Contrarily, during Cow pose (Right picture), the thoracic spine should extend without hyperextension in the lumbar spine. Cat/Cow Movement AnalysisDuring the Cow exercise (Right picture), a clear hinge point is noted in the junction between the thoracic and lumbar spines as indicated by the blue arrow. This hinge point occurs because the person cannot isolate the mid thoracic spine as she moves into the posture. If my intention is to improve thoracic mobility, and I do not correct this movement pattern, it becomes a bad exercise. With proper movement retraining- including engaging the Transversus Abdominus (TrA) and extending through the upper chest- she was immediately able to perform the movement correctly. During the Cat exercise (Left picture), the woman is unable to reach a uniform spinal curve. The lower thoracic spine remains flat throughout the motion with an inability to flex through the region. Movement retraining including focusing on pelvic mechanics and proper breathing, assisted in improving this pattern. Clinically, try not to get caught up on 'good versus bad exercises.' If it is addressing the patient's pain, minimizing their irritability level, and can be linked to a future functional activity, it is a good exercise. Remember, always focus on quality over quantity when it comes to prescribing movement. Jim Heafner PT, DPT, OCS Interested in learning more about Movement Analysis?  OPTIM recently launched The Movement Corner. The Movement Corner breaks down the complexities of human movement with video and picture analysis. We focus on analyzing functional movements and exercises, identifying common misalignments, and discussing why these misalignments typically occur. OPTIM is now enrolling the Dallas COMT!  OPTIM's COMT program is designed for the individual seeking to become an expert clinician. In our program, we provide a residency-type learning environment. Students will be exposed to quizzes, assignments, readings, lectures, and weekend labs. You will receive a residency level education and 75+ weekend lab hours. At the end of the program, you will be qualified to sit for the COMT examination as well as test into a fellowship program if you choose.
2 Comments
 I cannot stress enough the importance of thorough preparation prior to an interview. This preparation should include a wide range of topics including self reflection of strengths and weaknesses, a deep understanding of the program you are applying for, achievements of the faculty at the program, and most importantly 'why' you are applying for the program. While preparing for my Orthopedic Residency at the Harris Health System in Houston, TX, I studied common interview questions and personalized them to questions that would likely be asked during my interview. Next, I practiced each question in the mirror, with a friend, and with my clinical instructors. Since each program will likely have a combination of panel interviews and smaller side interviews, it is important to be well-rounded and dynamic in each environment. Interviewing is like public speaking. It gets easier and less intimidating with practice.Questions the program will likely ask the candidate1. Why did you apply for our program? Answering this question is your opportunity to show the interviewees that you have studied their program. In other words, this in the chance to explain why you are the unique applicant they are looking for! Your answer should highlight some of their specific programs features (i.e. journal clubs, local teaching opportunities, involvement in the local PT association). Do not be generic with this response! 2. What are your strengths and weaknesses? This is one of the most commonly asked interview questions. Know your top 3 strengths and top 3 weaknesses. The program wants to see if your strengths match the strengths of the program. Give personal examples regarding how you have lived out each of your strengths. More importantly, the program wants to see what steps you are actively taking to improve your weaknesses. 3. What are your short and long term goals? Having short and long term goals demonstrates that you have thought about your future. In my case, I made sure that my long term goals lined up with characteristics that the Harris Health System program would value. For example, I was applying for an Orthopedic Manual Therapy Residency. Therefore, one of my long term goals was to become an Orthopedic Manual Therapy Fellow as well teach Orthopedic PT across the country. Other common questions: 1. Explain a situation where you had to deal with a tough ethical dilemma. 2. Describe a time where you had a conflict with a superior/boss. How did you resolve this conflict? 3. How do you see the profession of PT evolving with the recent changes in government, healthcare, and PT reimbursement? Questions you should be asking the program1. How are the mentoring hours structured? How many 1-on-1 hours are spent each week working with a mentor? 2. Is the program currently conducting any research? 3. What is the pass rate of the prior graduates on their specialty examination? ==> This questions will show you if the program is adequately prepping their residents for the specialty exam. 4. What are the former graduates currently doing- Are they still working with the residency program? Are they involved in the APTA? ==> I find it a red flag if the program does not know where their graduates are currently working OR if none of the graduates are affiliated with the program. Final ThoughtsSpend quality time writing out answers to every potential interview question, then practice over and over! Additionally, be familiar with information regarding the APTA Core Values, APTA Vision and Mission Statement, and local state PT laws of the program that you are applying for. Residency and Fellowship programs are very competitive. In order to succeed you must identify the characteristics in yourself that differentiate you from the competition! -Jim Heafner PT, DPT, OCS  Interested in learning more from OPTIM COMT and Manual Therapy Fellowship Program? OPTIM is now enrolling it's Dallas Cohort! We structure our COMT program similar to an Orthopedic Residency. With 6 weekend courses and weekly online mentoring, our mission is to change your clinical practice!  Want to improve your clinical examination efficiency? OPTIM Faculty and author of this post, Jim Heafner PT, DPT, OCS, recently published 'The Guide to Efficient Physical Therapy Examination.' His ebook guides students and physical therapists through an efficient lumbar, cervical, shoulder, and lower quarter examination. Click HERE to BUY NOW! (Use promo code TSPT50 at checkout to save >$20!) People often ask me, "what are the best reasons to pursue a residency program versus start practicing immediately out of PT school?" While my answer often includes better manual therapy treatments, improved clinical reasoning and differential diagnosis, and improved patient education/ communication, the top answer I give all students is clinical efficiency. Clinical Efficiency: Arriving at the correct physical therapy diagnosis and determining the appropriate plan of care without performing unnecessary tests and measuresIn physical therapy school, therapists are taught a broad spectrum of knowledge. Orthopedic examination, treatment, and prognosis is covered in-depth. For example, we learn more than 50 special tests to diagnose various shoulder pathologies. Unfortunately, the majority of these special tests lack diagnostic reliability and rarely change our plan of care. Using the example above, if a 35-year old patient presents with left shoulder pain following a work injury, the clinician should be suspecting shoulder impingement, labral tear, rotator cuff pathology, AC dysfunction, among other diagnosis'. Assuming that the patient has negative rotator cuff tests and no gross loss of stability or strength, what is the benefit of performing additional tests for the labrum? One could potentially argue the need to further assess tissue irritability. Otherwise, the majority of these tests are fruitless.  Personally, this was a hard habit to break. I had learned all the special tests in school, and I was determined to practice them (I even recorded over 100 of them on TSPT website...) Upon finishing my clinical examination, I was drowning in information that only minimally changed my patient’s prognosis or intervention selection. With great mentorship at the Harris Health System, I quickly stopped this practice pattern and learned a much more efficient examination system. The new system shifted my thinking from a pathoanatomical approach (injured anatomy) to a movement dysfunction approach (poor movement).
Special tests are not bad as long as the individual performing them understands 'why' they are performing the test and 'what' implications the test has on other local structures. Ultimately, one should strive for an efficient movement based examination. -Jim Heafner PT, DPT, OCS OPTIM COMT Instructor  Interested in learning from OPTIM Manual Therapy? Now enrolling for our Dallas 2017 cohort. Please check out the OPTIM website if you are interested!
 Physical Therapy school prepares therapists to be general practitioners. Upon graduation, PTs are not experts in Orthopaedics, Cardiopulmonary, Geriatrics, or any specific subject area. There is simply not enough time! Due to a lack of classroom time, education focuses on the best current evidence, much of which is guided by pathoanatomy. To become an expert, we need to apply ourselves on a much further level. Below I have listed 2 clinical concepts that are not given adequate attention in Orthopedic Physical Therapy practice. Muscles can be dominant, but still weakMost people are trained to view muscles as either short and strong OR long and weak. Clinically, this is not always how muscles function. The upper trapezius is a classic example of muscle dominance with poor performance. The upper trap functions to upwardly rotate and elevate the scapula. The function of this muscle is especially important above 90 degrees of shoulder flexion. Due to scapular positioning, prolonged postures, and body composition, many people overactive the upper trapezius in lower levels of shoulder flexion (0-90 degrees). Consequently, the muscle becomes 'dominant' early in the range of motion. In these individuals the upper trapezius is actually weak in the functional range (above 90 degrees). When this muscle prematurely activates, it can lead to shoulder impingement syndrome or rotator cuff dysfunction. For this reason, it is important to retrain the upper trapezius in the functional range of motion. The upper trapezius is a single example of muscle dominance. Similar dysfunction can also be found in the hip flexors and hamstrings. Treat the joint first and the 'tight muscle' will resolve itselfThe joints are the gate-keepers to our other tissues. We cannot clear up muscle dysfunction or movement impairments if the joint is not moving properly. An example of this clinical reasoning is treating the thoracic spine with shoulder dysfunction. If a patient lacks upper thoracic extension or side bending, they will not be able to fully reach overhead. The hypomobility in the thoracic spine will limit rib cage expansion as well. If the practitioner only focuses on glenohumeral joint mechanics and scapular strength, they are not treating a major cause of the dysfunction. While the patient may make improvements, the long term solution to this problem is addressing the spine in conjunction with retraining the shoulder complex.  -Jim Heafner PT, DPT, OCS OPTIM COMT Instructor Jim is author of The Guide to Efficient Physical Therapy Examination & the Anatomy of Human Movement (an online movement resource). Purchase these products together & save nearly $40 (offer expirations 1/22/17)  Five years ago, I was diagnosed with right Venous Thoracic Outlet Syndrome. My 11-hour surgery entailed a first rib resection, subclavian vein graft, A-V fistula, and removal of my anterior and middle scalene muscles. Since the surgery, I have been doing great. I have resumed all activities with minimal shoulder pain or discomfort (as long as I perform routine corrective exercises for the shoulder girdle). I continue to have mild upper extremity swelling, which is gradually improving. My subclavian vein graft did not accept, so my collateral circulation has taken over. As my surgeon explained, "the main highway for blood transport is gone, so all the other side roads are taking over." Fast forward 5 years.... Four weeks ago I began experiencing right medial elbow pain with the sensation of swelling. Going through my differential diagnosis, I did not present with any symptoms of medial epicondylagia, very mild numbness and tingling, no neck pain, and no shoulder problems. The pain did not appear purely musculoskeletal, so I began getting nervous about the symptoms. After all, the last time I had right arm symptoms, the result was a 4" blood clot in my subsclavian vein. My brain immediately was flooded with thought viruses regarding potential causes of the problem.
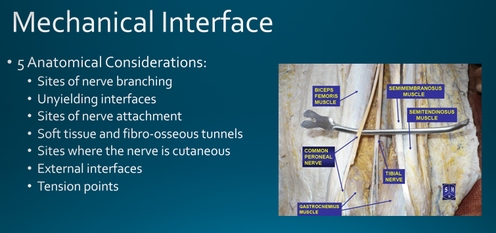
Image explaining potential causes of peripheral nerve entrapments In conclusion, the nervous system can create interesting signs and symptoms that may not appear musculoskeletal in nature. Additionally, always remember the patient's past medical history, recent change in activity status, and peripheral nervous system anatomy.  Interested in learning more about Peripheral Nerve Entrapments? The OPTIM online lecture series recently created a lecture on Peripheral Nerves. The lecture covers understanding basic nerve anatomy and function of the nervous system; identifying potential causes of peripheral nerve entrapments; differentiating between lower extremity nerve entrapment and lumbar radiculopathy; Demonstrating the ability to find, palpate, and treat lower extremity peripheral nerves dysfunction.  Author: Jim Heafner PT, DPT, OCS Jim teachers for the OPTIM COMT program in Scottsdale, AZ. He is owner of Heafner Health in Boulder, CO & one of the authors of The Student Physical Therapist Do your treatment sessions feel disorganized?Example 1: Do you prioritize therapeutic exercise or manual therapy first in your treatment session? The answer is manual therapy. If you are currently squeezing manual therapy into the end of a treatment session, STOP! The manual therapy needs to be performed early in the treatment so that changes in mobility or tissue extensibility can be sustained with motor control exercises afterward. Example 2: After your manual techniques do you choose to perform motor control exercises, power based movements, or strength training? and Why? The answer is motor control exercises. After a manual therapy technique has corrected a mobility deficit, we need to sustain those changes with motor control/movement retraining exercises. Once the motor control is achieved, then the patient can progress to power and strength based training. Feel free to download it and use it in your practice.
About OPTIM Our mission is to transform physical therapists into experts in neuromuscular examination and treatment. Originally based out of Houston, Texas, OPTIM now has instructors practicing in Arizona, Colorado, and Washington. We offer a Certification in Orthopedic Manual Therapy (COMT) and a Manual Therapy Fellowship (FAAOMPT). OPTIM hosts courses in: Houston, TX Scottsdale, AZ Dallas, TX (begins June 2017) St. Louis, MO (begins September 2017) |
Details
ContactEmail Good readsCategories |
||||||||||||






 RSS Feed
RSS Feed