The 2021 OCS exam is closer than you think!Studying for the Orthopedic Clinical Specialist (OCS) examination can be a tedious task and a bit overwhelming. Unlike the NPTE, many people who are preparing for the OCS have full time jobs, families, and other commitments to juggle. Plus, there are only a few high quality resources available to help one prepare for the exam and even fewer which provide practice quiz or test questions. For this reason, OPTIM has comprised a library of nearly 300 questions that can adequately prepare you the OCS examination! In this post, we will provide you with 5 questions that you MUST be prepared to answer while taking the OCS examination. With each question, consider the larger topic, background information, diagnostic accuracy (if appropriate), contextual factors, and more. **All answers provided at the bottom of this post! Question 1A 37-year-old female patient presents to you in clinic with complaints of low back pain that radiates down into her right hip and upper thigh pain that started two weeks ago after she picked up her 4 year old son and felt a “pop” in her back. She reports that immediately after the injury her back felt stiff, but by the time she woke up the next morning she had 5/10 pain on the R side of her low back that jumped to 9/10 and spread halfway down her right leg with forward bending. She reports that her pain might be getting a little bit better, but she still can’t bend forward without pain and that sitting or driving for more than a few minutes increases the pain significantly. She reports that her most comfortably position is standing or walking. Based on the treatment based classification (TBC) system which of the following is the best approach to physical therapy management for the patient in the case above? Select one: a. Traction b. Stabilization c. Specific exercise d. Manipulation Question 2A patient presents to you 2 weeks s/p FOOSH injury that occurred while she was in her yard raking and stepped awkwardly on a pine cone which caused her to fall down and brace her fall with her right hand. She reports pain in the right wrist that she assumed would go away on it's own but has persisted. Which of the following are signs that a patient may present with a scaphoid fracture and could warrant referral for further imaging to rule out a fracture? a. Palpation to the anatomic snuffbox b. Palpation of the scaphoid tubercle with wrist extension c. Axial loading of the first metacarpal d. All of the above
Question 3Which of the following tests are considered the most evidence based cluster for determining sub-acromial impingement?: Select one: a. Hawkins-Kennedy, Painful Arc, and ER MMT weakness b. Neer, relocation, and Hawkins-Kennedy tests c. Empty can, Hawkins-Kennedy, and speed’s tests d. Sulcus sign, speed’s test, and empty can test Question 4Which of the following MRI findings is an EARLY sign of disk degeneration? a. Reduced signal intensity in the nuclear area of the IV disc b. Disc space narrowing c. Osteophytes d. Spinal stenosis Question 5A patient presents to PT with complaints of numbness/tingling in the L antero-lateral thigh that impact standing and sitting comfortably. You find diminished sensation in this area however, motor performance is intact and the patient has full hip ROM. Which of the following health conditions should be at the top of your hypothesis list? a. Lumbar radiculopathy (L 4,5) b. Meralgia Paresthetica c. Sports hernia d. Trochanteric Bursitis Answers
4 Comments
IS it Clinically Appropriate to manipulate the Glenohumeral Joint?The glenohumeral joint is the most mobile joint in the body. Typically, joints that are very mobile do not require significant mobilization or manipulation; however, there are indications for a glenohumeral joint manipulation. The lateral manipulation (shown below) is a safe and effective technique to get improve GHJ mobility. Since it is a general lateral distraction manipulation, it can help improve mobility in multiple planes of motion. From a purely biomechanical standpoint, the examiner should expect improvements in horizontal adduction. Who is appropriate for this technique?Clinically, I have found the most success with lateral manipulations in patients who have adhesive capsulitis. These patients often have restrictions is multiple planes of motion and joint mobility is a primary impairment. Additionally, individuals with shoulder osteoarthritis, hypomobility, or end-range of motion restrictions are typically good candidates. Be sure to ask about past shoulder injuries prior to performing the lateral shoulder manipulation. If the client has any history of shoulder dislocations or subluxations, DO NOT perform this technique. Finally, be sure to address all of the causes of shoulder range of motion deficits as well. This includes assessing the thoracic spine, ribcage, scapulohumeral rhythm, and more! -Jim Heafner PT, DPT, OCS About OPTIM Manual Therapy? The current model of clinical education is insufficient. Unwarranted practice variation in our field is widespread and has enormous consequences. Our goal is to train the next generation of physical therapists to be expert clinicians in manual physical therapy. We strive to change the practice of physical therapy, develop leaders, and facilitate ongoing growth in physical therapist practice. OPTIM currently offers two programs, Certification in Orthopedic Manual Therapy (COMT), and a Fellowship in Orthopedic Manual Therapy (FAAOMPT). Click here to see a list of our course locations! In many instances, there seems to be a disconnect between the home exercises and pain/symptoms. The prescription of various exercises, movements, or education should be viewed as the missing piece to help keep a patient out of pain. However, patients often have a negative viewpoint of their home program. Either patients are not associating their home program with less pain OR therapists are not providing confidence that the home program is a significant key to success. Something needs to change! Why is the HEP Important?When I educate my patients, I specifically tell them that the home exercise program should become part of their daily 'movement routine.' For example, I recently was working with a cyclist who sits at a desk for 8+ hours each day. I told him as long as he is sitting for long periods of time and wants to continue to bike, he needs to be performing thoracic mobility exercises on a daily basis. The amount of available movement in his thoracic spine is significantly limited and his current daily activities are doing nothing to improve that state. The reason he is experiencing pain is due to a lack of movement diversity. The home exercise program ensures that patients are regularly performing movements that desensitize the nervous system and minimize any threat to potentially painful activities. We do so many things for maintenance every day! We brush our teeth twice a day, Shower, Eat healthy, SLEEP, etc... For some reason, basic movement is not a priority.Understanding HEP Frequency and DurationMost exercises are initially prescribed for pain management, mobility, or motor control.* Fairly quickly, the client's pain should decrease, the weak muscle should get stronger, and/or the joint should have more mobility. Once that goal is achieved, the home program can slow down. However, if one's life activities do not change, the same movement patterns will likely return and pain may return. With my clients, initially I often have them perform their HEP anywhere from 1x/day to multiple times per day until symptoms resolve. Once pain is managed and the patient's primary impairments improve, then I gradually wean clients down to a more manageable routine. The tipping point happens when the patient's activities change. Using the example above, if this cyclist started doing yoga or other flexibility exercises, then he would not have to perform specific thoracic mobility exercises. Until that point, he should perform those exercises regularly. While there is no magical formula for decreasing HEP frequency, I recommend that therapists view the HEP as a maintenance program that should be performed until the patient changes certain life activities. *If exercises are given for strength or power (low reps, high weight), the frequency should be adjusted. Typically strength and power is not given early in the plan of care. DO NOT THINK ABOUT THE HOME PROGRAM AS 'PHYSICAL THERAPY EXERCISES.' THINK ABOUT THE MOVEMENTS AS A DAILY MAINTENANCE PROGRAM. Redefining the Home Exercise programWhat do I mean by redefining the HEP? My intent is to change the focus, direction, and importance of prescribing the home program. Why? First off, who likes homework? Not many people. From a neuro-lingustic programming standpoint, homework has been engrained in our brains to be a negative, boring, and seemingly pointless activity. For this reason, it is imperative that during the therapy session each prescribed exercise be linked to a positive change in the patient's symptoms. In the OPTIM COMT and Fellowship programs, we demonstrate this positive change through the asterisk sign. The asterisk sign gives me the power to show my patients that the treatment (typically manual therapy + exercise) created a positive change in their symptoms. Doing more of that same treatment at home will get them better! Second, exercise! Not the most popular subjects in certain parts of the country. Selling exercise is like attempting to sell ketchup popsicles (thanks Tommy Boy!). Exercise is generally viewed as tough, sweaty, and painful. People often have many preconceived notions surrounding the fitness culture. Selling it is not an easy task. Finally, a program! Trying to instill a new program into someone's day is near impossible. People are highly resistant to change. If the home program is not accessible and easily understand, it will likely not be performed appropriately or at all. the Home Exercise Program requires adding something new into the patient's Day that is at their busy home, and requires physical and mental effort... No wonder we are not more successful!How to Prescribe a SOLID HEP 1. Be Concise
For me personally, I take videos of the patient performing all of their home exercises on their phone. In the video, I outline sets, repetitions, frequency, and common things to look out for.  -Jim Heafner PT, DPT, OCS OPTIM COMT Instructor About OPTIM Manual TherapyThe current model of clinical education is insufficient. Unwarranted practice variation in our field is widespread and has enormous consequences. Our goal is to train the next generation of physical therapists to be expert clinicians in manual physical therapy. We strive to change the practice of physical therapy, develop leaders, and facilitate ongoing growth in physical therapist practice.
OPTIM currently offers two programs, Certification in Orthopedic Manual Therapy (COMT), and a Fellowship in Orthopedic Manual Therapy (FAAOMPT). Click here to see a list of our course locations! Become a Specialist or NOt...That is the Question!Let's nip this question in the bud immediately. Yes, become a clinical specialist. Over the years, many people have questioned the need and/or benefit of becoming a physical therapy specialist. Common excuses include, "the exam material is outdated," "the exam does not test actual clinical knowledge,' among others. Put those comments to rest! If those are the only reasons to take the examination, then your probably doing it for the wrong reasons. Reasons to take a specialty examination: 1) Preparing for the examination requires months of studying and delving into a specific subject matter. It requires focus and dedication. 2) The exam material covers the highest quality research in the field (typically minus the last 12 months of research). This may be slightly different from daily clinical practice, but it is the best we have! 3) Become recognized as a regional expert in the field. 4) Studying each topic will allow thorough reflection regarding what is right and wrong with current clinical practice. Are you interested in becoming an Orthopedic Clinical Specialist (OCS)?Below is information regarding the OCS Examination. The examination is hosted by the American Board of Physical Therapy Specialists (ABPTS). (Since my background is in Orthopedics, I am writing on the Orthopedic examination. Please note that these steps and links will take readers to all specialty fields.) Important dates for the 2018 Examination:
Last year the application deadline was July, 31st. Follow this link to learn more about the Orthopedic test. Once the application process begins, this link will have an online application link. Who is eligible to apply for the examination? "Eligible clients must:
The above information was taken from the 2017 OCS Exam Candidate Guide.  Want a program that has BOTH the clinical and didactic skills to prepare you for your speciality exam? Check out OPTIM Manual Therapy. OPTIM offers both a Certification in Orthopedic Manual Therapy (COMT) and Fellowship in Manual Therapy (FAAOMPT)! We emphasize current best evidence into clinical practice including paradigms like utilizing a bio-psycho-social approach, leveraging patient expectations, and purposeful interventions to provide excellent clinical outcomes. Currently, OPTIM offers courses in Houston TX, Dallas TX, Scottsdale AZ, and St. Louis MO (coming this September!) 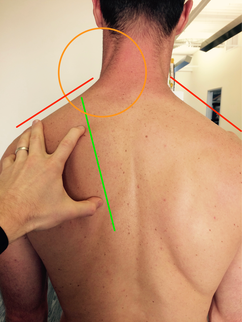 Scapular Depression Syndrome with associated Scapular Downward Rotation Scapular Depression Syndrome with associated Scapular Downward Rotation I was recently treating a patient who presented with left shoulder pain, weakness, and the sensation of instability following a surfing accident. The patient denied any history of dislocations, but reported the shoulder felt weak 'as if it could pop out' in various overhead positions. Due to the traumatic onset of symptoms, I suspected a partial labral tear or rotator cuff involvement as the underlying pathoanatomical problem. Regardless, it is not my job to fix the anatomical issues. As the physical therapist, it is my job to treat his underlying impairments and provide education on pain and proper movement. At his initial evaluation, he had both static and dynamic postural deficits. Statically, he was resting in scapular depression and downward rotation (see picture to the left). Dynamically, he had limited overhead mobility (see video below) as well as weakness in his serratus anterior and upper trapezius muscle. Additionally, he had decreased cervical rotation range of motion due to the depressed position of his scapula. A 'scapular assistance test,' which provides support to the shoulder girdle, revealed full, painfree cervical range of motion.
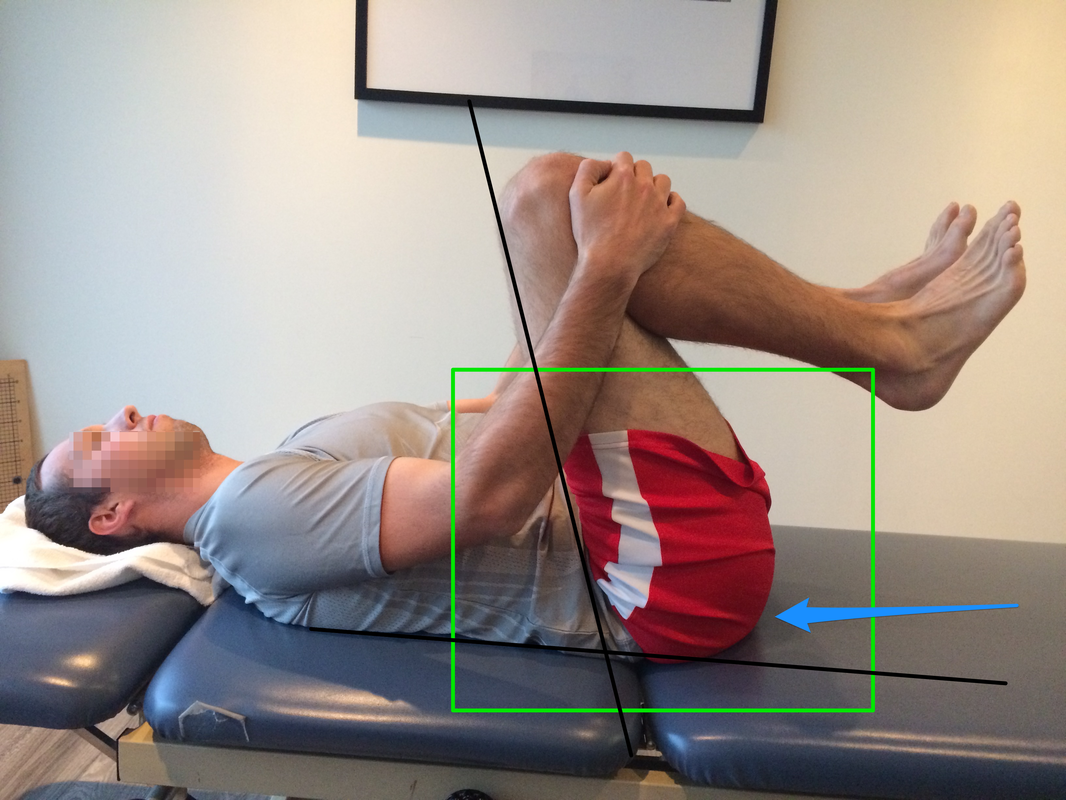
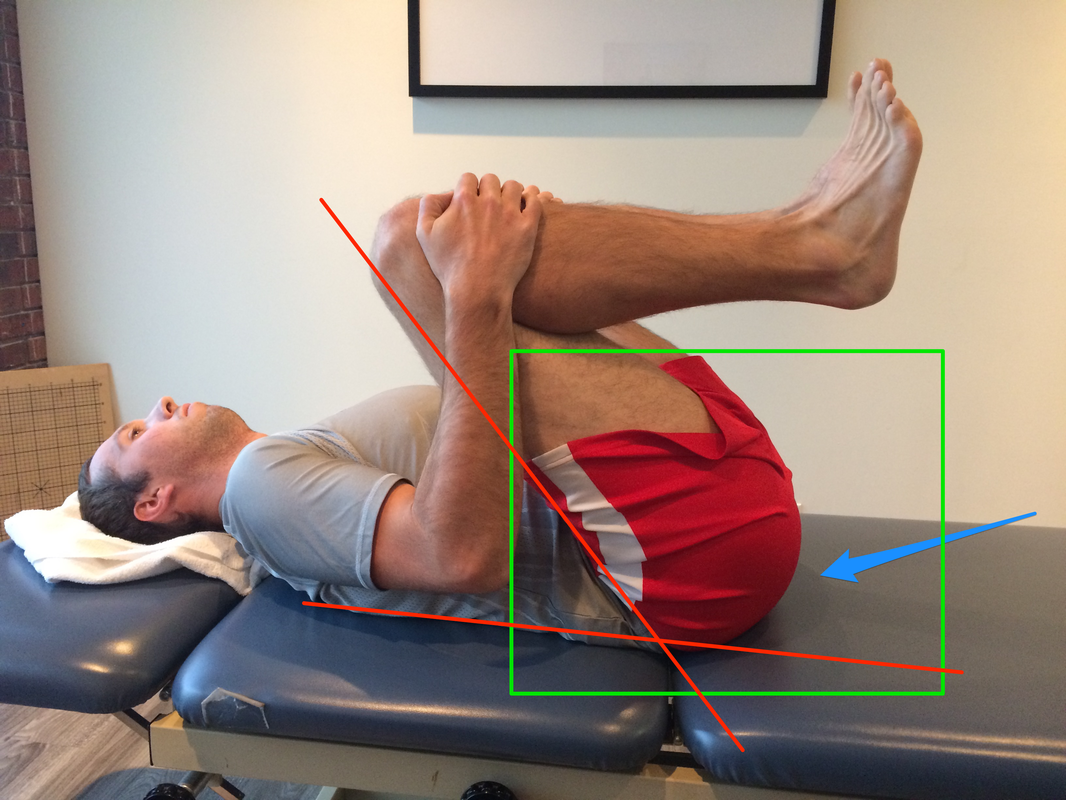
As part of his plan of care, treatment focused on retraining the upper trapezius muscle. Prior to starting therapy, his upper trapezius was placed in a chronically lengthened position due to his resting scapular posture. When reaching overhead, the upper trapezius muscle would activate early in the range of motion, and it could not complete its role as an upward rotator. The glenohumeral joint was placed on extra stress because the scapular stabilizers were not working synergistically. These deficits resulted in a sense of instability when reaching overhead. Strengthening or retraining the upper trapezius is typically important in individuals with a scapular depression. Identifying the movement dysfunction and addressing the proper impairments can prevent a patient from having surgery or prolonged pain. Jim Heafner PT, DPT, OCS  Want to learn more about dysfunctional movement? Check out OPTIM's Movement Corner, which focuses on deconstructing how and why we move! Sign-up before 12/14/16 and receive a complimentary copy of Dr. Heafner's Ebook, The Guide to Efficient Physical Theray Examination ($42 value).  OPTIM's COMT program is designed for the individual seeking to become an expert clinician. In our program, we provide a residency-type learning environment. Students will be exposed to quizzes, assignments, readings, lectures, and weekend labs. You will receive a residency level education and 75+ weekend lab hours. At the end of the program, you will be qualified to sit for the COMT examination as well as test into a fellowship program if you choose. Hip flexion is necessary to complete a squat, forward bend, or even initiate the swing phase of gait. Whether the movement is open-chain or closed-chain, proper timing and activation of the hip flexors as well as disassociation of the lumbopelvic region is essential. Normal hip flexion active range of motion should be ~120 degrees. Due to prolonged sitting and chronic lumbar flexion posturing, many individuals lack adequate hip flexion. As a compensatory strategy, these people will move into early lumbar flexion when attempting hip movements. When assessing hip flexion in the clinic, first I have the patient perform the movement without any cueing (R picture above). During this assessment, I look to see if the individual can disassociate the low back from the hips. As one can see, this person does not perform an isolated movement. As he pulls his femurs towards his chest, he rolls off his sacrum into a posterior pelvic tilt. The right image portrays both hip flexion and lumbar flexion. The left picture demonstrates his actual hip flexion range of motion. This range of motion is significantly less than the motion depicted on the R image. From a subjective complaint, he also reports a pinching pain in the anterior hip with this movement. The movement has shifted from appearing functional to very dysfunctional simply by cueing the position of the tailbone.
Identifying movement compensations is a topic I discuss frequently on The Movement Corner. In physical therapy school, we learn about kinesiology and regional interdependence, but we do not spend enough time viewing dysfunctional movement patterns. We know the body is one connected unit, yet we often forget this concept when prescribing exercises or looking at natural movement patterns. Identifying these dysfunctions will make you a more efficient clinician. -Jim Heafner PT, DPT, OCS |
Details
ContactEmail Good readsCategories |




 RSS Feed
RSS Feed