 It appears that Move Forward PT collaborated with Dr. Oz on their most recent segment: Could that pain be your unhealthy fascia? Before listening to the podcast, I prayed that it would be a 5 second segment with a long drawn out, "NOOOOOOOO!!!" Unfortunately, it was 23 minutes, 53 seconds of discussing fascia, how it is injured, and how the fascia can inhibit movement. In one segment, the interviewee Mary Ann Wimarth PT, DPT, OCS discusses a patient example who benefited from myofascial release of the iliotibial band with part of her home program being foam rolling of the IT band. At OPTIM, I say Mary is likely neglecting the cause of the dysfunction. The IT band cannot be lengthened. It is a taut, fibrous band of connective tissue. Did Mary investigate the mobility of lumbar spine, hypertonicity in the hip flexors, gluteal muscle strength, and how the core is functioning during a functional assessment? I am not sure. If the IT band is suspected to be "tight," I would perform an Ober's test. If the Ober's test is positive, investigate hip strength, hip flexor length, and the L4-S1 segments (since the TFL is innervated by L4-S1 and is the origination of the IT band). If the lower lumbar spine is not moving properly, I would choose to manipulate that region to provide a neurological reset and decrease any hypertonicity in the hip flexor musculature. The HEP would consist of more active hip and core motor control exercises, and less passive foam rolling. My final grievance with this segment is the timing of which a consumer should seek physical therapy. Mary states that a person should try the foam roller for a while if they are having symptoms. If the foam roller does not work, then the consumer should receive an assessment from a physical therapist. The order is backward! If someone is having pain, they should go to a physical therapist first. Physical therapists are the front line of defense for musculoskeletal dysfunction. As movement specialists, we can evaluate the cause of one's dysfunction, then give appropriate management. Do not believe everything you read! -OPTIM Manual Therapy Fellowship
2 Comments
 Some people say the SI Joint does not move. The Sacroilibat (seen here) disagrees! Studies have shown that the Sacroilibat actually frowns when it needs to be manipulated. Check out our OPTIM youtube video below regarding how to perform a manipulation for a posterior rotated ilium. Hope you enjoy the Thursday humor, OPTIM Manual Therapy Fellowship  Have you ever had difficulty discussing chronic pain with your patients. In this post, Todd Hargrove breaks down chronic pain in simplistic terms. If posts like this interest you, check out OPTIM Manual Therapy Fellowship, which dedicates over 16 hours of lab and lecture to pain management and the biopsychosocial aspects of patient care. A Systems Perspective on Chronic Pain Very interesting thoughts from Peter O'Sullivan. We completely agree that the cognitive aspects of low back pain cannot be ignored. Rotation is the primary motion that occurs at the atlantoaxial joint (C1-C2). Normal rotation at this joint is ~38 degrees to either side. To assess for C1-C2 dysfunction to the right (for example), fully sidebend the head to the left, then fully rotate to the right. The sidebending component locks out the lower cervical segments and prevents these segments from rotating. -Note: when novices are practicing this manipulation, a loss of sidebending is generally the reason the manipulation is not successful. Make sure to maintain the sidebending component while rotating the head. -Practice tip: to improve speed with cervical manipulations, practice by using a pillow. *we know the video is titled CT Supine, we are changing it.* 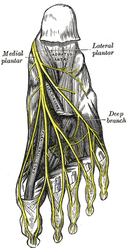 One of the key components of our fellowship program is differential diagnosis. Appropriately identifying the cause- the body system and specific structure involved- of a patient's symptoms is essential. Recently The Student Physical Therapist wrote a great post discussing plantar fasciosis versus lateral plantar nerve pain. We could not agree more this post. At OPTIM, we have seen multiple patients who responded well to 'typical' plantar fasciosis treatment (corrective exercises, shoe inserts, lifestyle modification), but something was missing. Addressing the neural symptoms has been that missing component in the treatment of many of these patients. Check out their post here! For more videos of manipulation and other great physical therapy information check out the OPTIM Facebook page and Youtube channel! |
Details
ContactEmail Good readsCategories |
 RSS Feed
RSS Feed